Adapting Emergency Ventilators for COVID-19 Patients
Detailed instructions and how-to videos are available online
When it comes to treating patients with COVID-19, there is a big difference between a crude emergency ventilator and a highly sophisticated hospital ventilator.
COVID-19 patients typically need higher pressures and more safeguards than an emergency ventilator can provide. But, in times of dramatic ventilator shortages, patients could be put on these simpler machines out of sheer necessity.

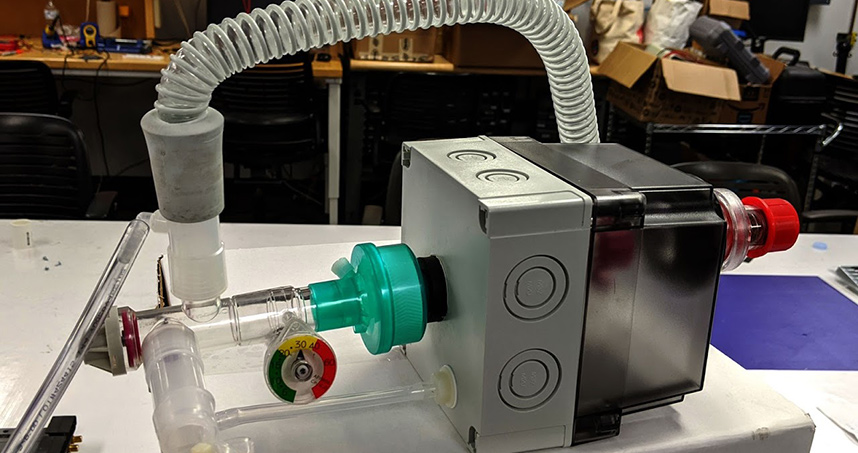
Now a team from Northwestern Engineering has found a way to retrofit a common commercial emergency ventilator (Vortran Go2Vent®) into a device better suited for COVID-19 patients. The device can reach higher inspiratory and end-expiratory pressures and gives physicians the finer, variable control needed to ensure the patient will not experience lung damage.
While this solution cannot replace hospital-grade ventilators, it could provide a quick fix in times of desperate need around the world. Instructions and videos for how to retrofit a Go2Vent are available online.
“We spoke with a doctor who explained that his hospital had 20 sterile Go2Vent® units available, but that COVID-19 patients seem to require significantly higher pressures than this ventilator is designed for,” said J. Edward Colgate, who co-led the work. “We were inspired to develop a simple, low-cost modification that extends the operating range of those devices.”
“There is a misunderstanding that a ventilator is a gadget that just pumps air in and out of a patient’s lungs, but some ventilators can do more harm than good,” added Michael Peshkin, who co-led the work with Colgate. “An ICU ventilator is a finely tuned machine, and the respiratory parameters are closely adjusted by physicians. If emergency ventilators are needed, we can give doctors more latitude in the available settings. Our solution can be used in a pinch, but we’re not aiming to substitute for ICU ventilators.”
Colgate and Peshkin are professors of mechanical engineering in the McCormick School of Engineering.
“Professors Colgate and Peshkin built a solution that not only meets clinical needs but could be rapidly produced with very easily obtained parts,” said Mozziyar Etemadi, a Northwestern Medicine anesthesiologist and research assistant professor at McCormick and Northwestern University Feinberg School of Medicine. “If we needed to use this, we absolutely could. And it would serve our patients in this difficult time.”
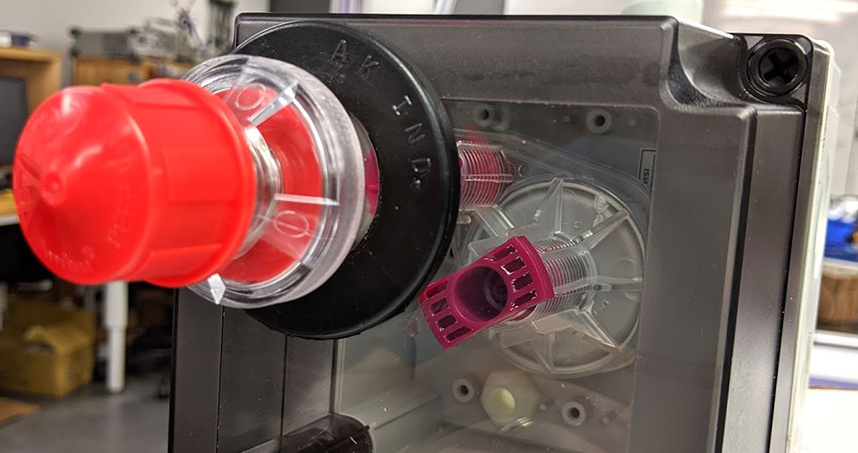
To adapt the emergency ventilator to reach higher pressures, the Northwestern team enclosed the Go2Vent® inside an airtight chamber with elevated pressure levels. They included a manually adjustable pressure-relief valve to maintain a constant pressure inside the enclosure. The team tested its retrofitted device, called the Pressure++ Project, on a lung model in the laboratory.
“The Go2Vent® continues to cycle as it normally does, and no modifications to its internal mechanism are needed,” the team said on their site. “All of its operating pressures are incremented by the ‘apparent’ atmospheric pressure that it is exposed to, which is slightly higher than actual atmospheric pressure.”
Because emergency ventilators also lack monitors and alarms, Colgate and Peshkin added features to the Go2Vent® that can monitor and display patient respiratory parameters. If a patient receives too much pressure, then an alarm can alert the physician. The team also is working on an alarm for slowed or ceased respiration.