Practical Solutions for a Healthier World
Northwestern industrial engineers work to make healthcare delivery more efficient, more reliable, and safer.
Time can mean life or death when receiving the life-saving organ gift from a deceased donor. Within a very narrow window, the medical team must preserve, transport, and match the organ with a compatible recipient. Any glitch in the system could lead to a wasted kidney or worse yet, a tragic outcome for the intended recipient.
Faced with an optimization issue like this, medical professionals can turn to the experts: faculty from Northwestern Engineering’s Department of Industrial Engineering and Management Sciences, who use data science to make complex processes more efficient and reliable.
Transplantation optimization is only one of many healthcare delivery challenges that faculty and students at the McCormick School of Engineering work to solve. These researchers also develop new ways to disrupt supply chains for counterfeit medications in low- and middle-income countries. The results of that effort could save lives and lead to new policies to protect the most vulnerable.
Optimizing Transplantation Systems
To produce optimal outcomes, kidney transplantation systems require a complex mix of medical and logistical procedures to be completed quickly, efficiently, and skillfully. With the greatest speed possible, a medical team must harvest the organ, determine how suitable it is for transplant, find the right donor, and deliver it there—a process mired in protocols and hampered by geography.
The potential implications for improving the process are big. In 2021, according to OrganDonor.gov, 90,483 people needed a kidney transplant. Only 24,670 received one.
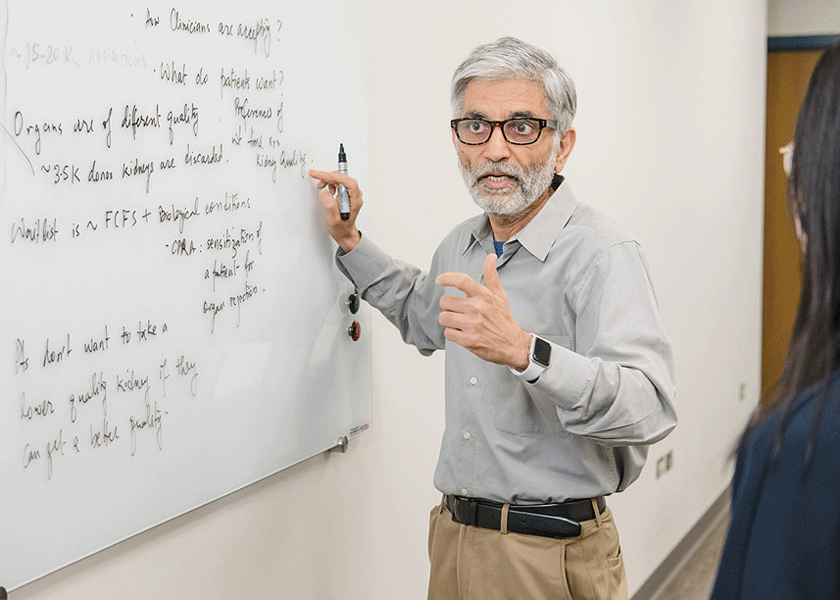
Professor Sanjay Mehrotra uses analytical modeling, data science, and machine learning to optimize kidney transplantation systems by creating new processes to determine which organs are suitable for transplant and who the best recipient will be. With colleagues from Northwestern Feinberg School of Medicine, the RAND Corporation, Duke University, and Yale University, he hopes to change the transplant system in the United States, making it more efficient while wasting fewer donated organs.
In an effort funded by the National Institute of Diabetes and Digestive and Kidney Diseases, Mehrotra collaborates closely with individuals who have held leadership roles at the United Network for Organ Sharing (UNOS), the national organization that seeks to develop policies and procedures that improve the organ transplant and donation process. The final deliverable of this patient-centered project will be a scientifically validated policy structure that over five years could save 5,000 to 7,500 lives from among the nearly 100,000 patients on dialysis waiting for a kidney transplant.
“You cannot pass every kidney that is donated through the same protocol, because that results in delays that would be unfair to the patients,” says Mehrotra, professor of industrial engineering and management sciences and director of the Center for Engineering and Health. “We need to figure out quickly who would benefit the most from the kidney because any delay could be dangerous for the patients.”
The research will help guide discussions at UNOS. The project has also aided in identifying some deeply hidden scientific problems on which no prior modeling or mathematical research has taken place. For example, machine learning could help healthcare professionals find ways to identify kidneys that will get discarded due to system inefficiencies, and optimize the life of the kidneys once they are harvested. Using the information gleaned from past transplants, scientists could determine which donor characteristics are most associated with successful procedures, the ideal temperature for storing the kidney after harvesting, the maximum time and distance a kidney can travel before implantation, and other key considerations.
Mehrotra is uniquely equipped for this kind of work. An expert in methodologies for decision-making under uncertainty and their application to problems in health systems engineering and other operations research applications, he can approach issues with an analytical grounding while looking for a way to optimize a crucial process.
“Kidneys are a finite resource that we need to maximize,” he says.
Disrupting Potentially Lethal Supply Chains
While industrial engineers often focus on efficiently moving goods to where they are needed, those same engineers can work to halt movement when necessary.
The World Health Organization estimated in 2017 that at least one in 10 pharmaceuticals consumed in low- and middle-income countries is either substandard or falsified, resulting in mortality estimates ranging from the hundreds of thousands to millions. One example of a vulnerable population is young children in sub-Saharan Africa in areas with high malaria prevalence.

As a PhD student in industrial engineering and management sciences, Eugene Wickett has taken to tackling this problem. After graduating in industrial engineering from Georgia Institute of Technology, he was building local health data infrastructure in Liberia when he saw the potential for more impact. He joined the PhD program at Northwestern in 2017 to study operations research for social good. Wickett has been designing methodology to solve these problems under the guidance of Karen Smilowitz, James N. and Margie M. Krebs Professor in Industrial Engineering and Management Sciences, and Matthew Plumlee, assistant professor in industrial engineering and management sciences.
Wickett’s research focuses on ways to disrupt the flow of degraded, poor-quality, or counterfeit versions of medications such as amoxicillin and antimalarials to hospitals and pharmacies. While on a related visit to Liberia in 2019, he spoke with regulators, pharmacy owners, and other stakeholders. Wickett began thinking about modeling the generation of poor-quality medicines in supply chains.
Several low- and middle-income countries conduct post-market surveillance. Through this process, products can be labeled as “substandard” if they have less than the usual amount of an active ingredient, or “falsified” if they are fake. Wickett has found that it is critical to understand the interaction between supply chains, which determines how the product arrived at a location, and post-market surveillance. This can help regulators to determine whether medicines have degraded under suboptimal storage conditions, were manufactured poorly, or were damaged somewhere between the manufacturer or point of use.
“Using supply-chain information, we can narrow down likely explanations for where products degraded, which aids regulators in targeting their intervention resources,” Wickett says.
Wickett is working to improve this process by combining on-the-ground pharmaceutical regulation with scientific procedures. That involves determining strategic priorities, deciding on when and where to sample medications, and identifying how best to analyze what was found.
“We need to be certain our approaches are useful for practical implementation,” Wickett says. “These statistical techniques can help regulators extract more utility from limited resources.”
Photography by Jason Brown and Matthew Allen
